Background: CBL proteins are a family of RING finger (RF) E3 ubiquitin ligases that regulate proliferative signals via ubiquitination and degradation of tyrosine-phosphorylated signaling protein ( e.g., FLT3, JAK2, MPL). Thus, the loss of CBL activity due to hypomorphic or loss of function (LOF) mutations functionally may result in oncogenic effects. However, simple LOF does not explain the high rates of c-CBL (most abundant CBL isoform, located on chromosome 11)missensemutations affecting a canonical position in the RF domain, catalytic region responsible for ubiquitin ligase activity.
We hypothesized that studying the molecular and clinical associations of c-CBL mutations will help clarifying the consequences of its mutations and conceptualize innovative treatment strategies.
Methods: We analyzed molecular and clinical features of a cohort of 11036 patients with myeloid neoplasia (MN; 63% AML, 29% MDS, 5% MPN/MDS, 3% MPN) from The Cleveland Clinic Foundation and public series. Clonal burden of c-CBL was analyzed to infer clonal hierarchy and to establish founder vs secondary mutations based on our previously described criteria.
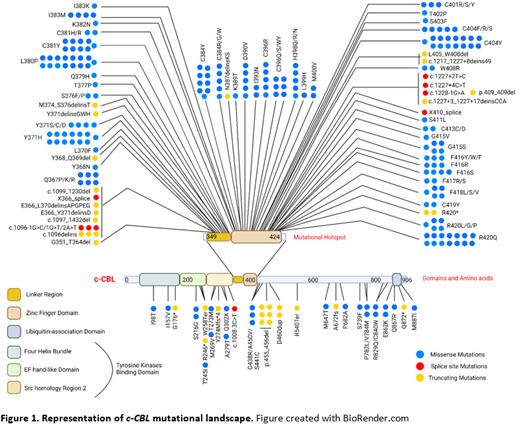
Results: Overall, c-CBL mutations were detected in 2.4% (270/11036) of the patients. The most common c-CBL mutations were missense (80%) and mainly occurred in the RF domain and linker region (83% of mutations, Fig1).
c-CBL mutations were found in 2% of both primary AML (pAML; 3% of CBF) and sAML/HR-MDS and 8% of CMML. Among CMML patients, mutations were associated with low-risk features (7% of CMML2 vs. 13% of CMML1). The most frequent co-associated mutations were TET2 (22%) and RUNX1 (19%) in all AML, ASXL1 (50%), SRSF2 (25%) and TET2 (25%) in MDS, and ASXL1 (50%), SRSF2 (44%) and JAK2 (28%) in MPN and MPN/MDS.
In terms of associations with tyrosine kinase receptors ( FLT3, c-KIT, CSF3R, c-MPL), we found that 18% of c-CBL mutants carried at least one mutation in one the four receptors, contrarily to what expected from previously reported results of c- CBL/FLT3 mutational exclusivity.
In most of the cases, c-CBL mutations were subclonal (53%), arguing against its primary driver/initiator function. Indeed, we observed c-CBL mutations as the only lesion in 7% of the cases with no specific disease association (66%, AML; 25%, LR-MDS; 8%, CMML).
There was no difference in MN phenotypes between carriers of canonical vs non canonical c-CBL mutations; however, we found that non canonical mutations were more often ancestral or the only founder lesion detected compared to canonical mutations (46 vs 31%, P = 0.031).
Del(11q) or monosomy 11 were found in 8 patients, without association with c- CBL VAF >50%. Furthermore, c-CBL VAF>50% was not associated with marrow blast infiltrate, WBC or shorter survival.
We then analyzed the effect of c-CBL in cooperation with RAS genes ( NRAS, KRAS, PTPN11, NF1) and found that, in AML, the effect of c-CBL with 2 RAS genes (5 patients, 3%) showed some trends toward higher blast count ( P = 0.079), higher WBC ( P = 0.076) and lower rates of normal cytogenetics compared to the effect of the remaining c-CBL mutant (0 vs 48%, P = 0.061).
Conclusions: In sum, our study of the molecular landscape of c-CBL mutations highlights that these lesions occur mainly during disease development with majority of the cases carrying subclonal hits with a weaker effect on disease phenotype and prognosis. Such mutations can be present in both primary and secondary AML (in contrast with previous reports) and additive effects can be observed when c- CBL mutationsco-occur with more than one RAS gene in these disease groups. In some cases, especially in non-canonical mutations, c- CBL could also act as ancestral event and as an independent leukemic driver.
Disclosures
Maciejewski:Omeros: Consultancy; Alexion: Membership on an entity's Board of Directors or advisory committees; Regeneron: Consultancy, Honoraria; Novartis: Honoraria, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal